Cancer Pain
Cancer Pain
Pain in cancer may arise from a tumor compressing or infiltrating nearby body parts; from treatments and diagnostic procedures; or from skin, nerve and other changes caused by a hormone imbalance or immune response. Most chronic pain is caused by the illness and most acute (short-term) pain is caused by treatment or diagnostic procedures. However, radiotherapy, surgery and chemotherapy may produce painful conditions that persist long after treatment has ended.
The presence of pain depends mainly on the location of the cancer and the stage of the disease. At any given time, about half of all people diagnosed with cancer experience pain, and two thirds of those with advanced cancer experience severe pain that adversely affects their lives.
With competent management, cancer pain can be well controlled in about 80% to 90% of cases. But despite all the resources, nearly 50% of cancer patients in the developed world continue to have poorly controlled pain. Worldwide, this number is more than 75%.
WHO has published guidelines for cancer pain management. Improved pain management may improve quality of life, but in some cases also prolong life.

Cause
Tumor-related
Tumors cause pain by crushing or infiltrating tissue, triggering infection or inflammation, or releasing chemicals that make normally non-painful stimuli painful.
Invasion of bone by cancer is the most common source of cancer pain. It is usually felt as tenderness, with constant background pain and instances of spontaneous or movement-related exacerbation, and is frequently described as severe.
When tumors compress, invade or inflame parts of the nervous system including nerves, they can cause pain and other symptoms.
Pain from cancer of the organs such as the stomach or liver, pancreas cause visceral pain that is diffuse and difficult to locate, and is often referred to more distant, usually superficial, sites.
Other causes of pain in cancer include treatment and infection.
Management
Cancer pain treatment aims to relieve pain with minimal adverse treatment effects, allowing the person a good quality of life and level and function and a relatively painless death. With skill and patience most cancer patients can have good pain control.
Cancer changes over time, and pain management needs to reflect this. Several different types of treatment may be required as the disease progresses. Health professionals should clearly explain the cause of the pain and the various treatment possibilities. These include psychological options, spiritual considerations etc. Other options include medications, life style modifications, various interventions, including placement of intrathecal pumps.
Patients whose pain cannot be well controlled should be referred to pain management or palliative care.
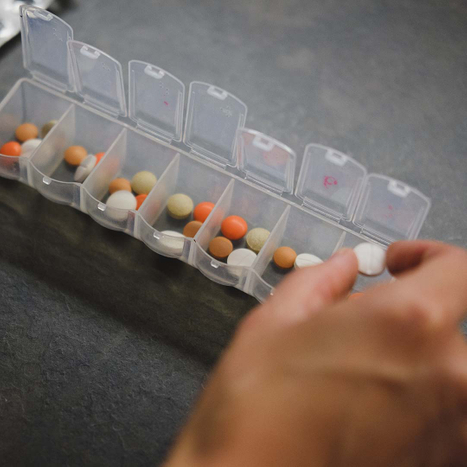
Medications
The WHO guidelines recommend prompt oral administration of drugs when pain occurs, starting, if the person is not in severe pain, with non-opioid drugs such as acetaminophen and non-steroidals. If adequate pain relief is not achieved, mild opioids such as codeine, or tramadol can be added. If necessary stronger opioids such as morphine, oxycodone can replace mild opioids, while continuing the non-opioid therapy. Dose of opioids can be increased to achieve pain control. Side effects may limit the dose escalation. In some cases presentation maybe with severe pain. Modifications of treatment protocol maybe necessary.
About 50% patients with advanced cancer and pain will need powerful opioids, and in combination with other adjuvant medicine can produce acceptable analgesia in 70–80% patients. Side effects of medications include nausea, constipations etc. These need to be addressed. Occasionally changing opioids maybe very helpful.
Based on symptoms, medications can be taken as needed or a combination of around the clock and as needed. As the diseases progresses, pain becomes more constant, and then around the clock medications need to be included in the plan.
Plan for pain management should be simple safe and effective. Oral medications are well tolerated, easily available and very effective. This should be the first choice of treatment, no matter the medication. There is no best analgesic. It is important to remember to add adjuvants to treat side effects, and potentiate the effects of analgesics.
Interventional
Various interventions can be used in combination with medications to control pain
Radiation
Radiotherapy is used to control the pain of a growing tumor, such as in bone metastasis (most commonly), penetration of soft tissue, or compression of sensory nerves. Relief may occur within a week of treatment and may last from two to four months.
Neurolytic block
A neurolytic block is method of reducing pain by interrupting the flow of pain. These interventions cause degeneration of the nerve's fibers and temporary interference with the transmission of pain signals. There are various methods of performing neurolytic blocks and in various parts of the body. Occasionally a block is performed with local anesthetic before a neurolytic block with alcohol, phenol etc. Surgical resection of nerves is not recommended. Because nerves often carry both sensory and motor fibers, motor impairment is a possible side effect of neurolytic block. Common neurolytic blocks performed include celiac plexus block for pancreatic cancer, intercostal neurolytic block for post thoracotomy and post mastectomy pain syndrome and superior hypogastric plexus block for pelvic perineal pain. Intrathecal neurolysis is an option in very carefully selected patients.
Targeted radiofrequency ablation and vertebral augmentation for spinal tumors.
This is a minimally invasive procedure where a needle is inserted into the affected vertebra and radiofrequency ablation using heat is performed to burn out the tumor. This is then followed be administration bony cement. After the procedure, it is hoped that there is a decrease in tumor load, stability of spine and reduction in pain.
Patient-controlled analgesia
Some times patients are not able to tolerate medications orally. This maybe after surgery, or in the case of patients with severe nausea and vomiting. Use of a patient-controlled analgesia pump, allows for pain control to be maintained via the intravenous route. Use of epidural patient-controlled analgesia is also an option in selected patients.
Intrathecal Pump
In some patients with advanced cancer with uncontrolled pain, chronic cancer related pain, or patients with significant opioid related side effects with poorly controlled pain, this is a very effective option. It is possible to achieve improved pain control with reduced side effects. This is done using a combination of medications. In addition, it reduces the need for oral medications. A personal therapy manager is used in combination. That gives significant flexibility and allows for rapid titration and control of pain.

Barriers to Treatment
It is important to understand that not all patients who have cancer will complain of pain. But more than 50% of patients with advanced cancer will complain of pain and majority will have poor pain control. There are multiple factors that have been identified, among them lack of education on pain management among providers, patient’s reluctance to discuss pain during visit with doctor, reluctance to take pain medications, availability of trained physicians, etc.
The evidence does show that with patience and understanding, seeking help when needed, most patients with cancer related pain can have good pain control.
